Psychedelics, Somatics, and an Ironman
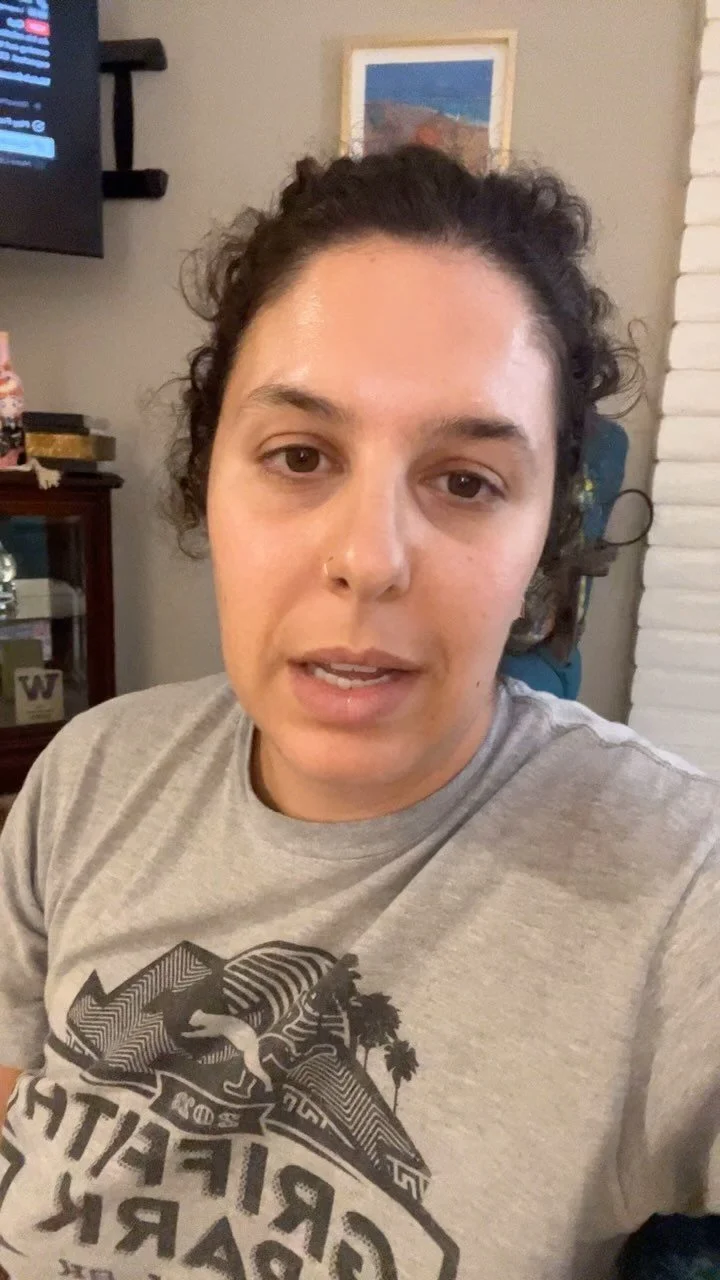
I share about my past year's journey towards completing my first Ironman!
About 1 year ago, I felt myself building a cocoon. I knew I was journeying inward and would need to retreat from others for this inner-exploration and work. Because I grew up feeling that my existence was about giving, and caretaking— focusing my attention inwards felt dangerous and defiant. I wasn’t sure my relationships could survive a time when I had little to nothing to give. And this unknown, is exactly what would lead me to healing this deep, inner-wound.
Around this time I made two choices that would be absolutely pivotal in my journey—
1) I began psychedelic-assisted Somatic therapy.
2) I began training for the California Ironman 2024.
See below some videos and photos from my year of training for the IRONMAN.
The Ironman training helped me be in my body throughout the trauma of my Mom’s death. It reminded me that an elevated heart rate is nothing to be afraid of. It reminded me that my body is alive and capable of changing. It gave me tools for managing stress hormones like cortisol. It taught me about fueling my body with nutrition and sleep. I learned to feel into the difference between my inner-intuition-voice and my inner-trauma-response-voice. While building strength and endurance, I also prioritized restoration in foam rolling, cold plunges, Yin and Nidra yoga. It helped me stay structured in my commitment to my body— it guided me through intense resistance, collapse and despair. I felt the density of my flesh and the expansiveness of my lungs.
There is a fear of mortality that is common amongst survivors of family-members who die from terminal disease. When Western Medicine says, “the likelihood of a person developing any kind of cancerous brain tumor is less than 1%",” some of us have experienced being the 1%. Relief of statistics just kinda goes away. In the year and half between my Dad’s death and my Mom’s death, I underwent 2 sleep studies, 1 echocardiogram, 1 cardio-stress test, 3 asthma attacks that lead me to urgent care, and many blood labs. I felt my heart more. I felt my lungs more. And I felt my heart break and was absolutely convinced I was having a heart attack. Turns out— it was all somatic and my heart is very much alive and well. The Ironman Training helped me trust that I could survive and even build capacity in the very real experience of so much pain. I also want to acknowledge my privilege in having access to medical diagnostic testing.
Also to name, Heart Disease in women is an important topic to talk about as symptoms present differently. You can read more here.
Psychedelic Somatic Therapy has absolutely changed my life. It allowed me to access traumas in my body that I never thought I could reach. Through this modality, I have dropped into the Self in such a profound way that I would describe the journey as an Ego Death. It feels like the parts of me that existed merely to survive my parents, are finally getting a chance to lay to rest. The part of me that felt relationships and connection extended only as much as I could give care, are softening so that I can rest in receptivity. There is healing in the give and take that is relationships. In somatic words, I am de-thawing and softening. Which is always an act of deep liberating freedom.
There is much more I could share in this experience that I will leave for another time including how this inner-journey intertwines with collective liberation— especially given the timing of my cocoon with my and Western world’s awakening to the many Genocides globally, including Palestine, Sudan, Congo. This deserves my focus in writing about for another time. But, what I do want to convey is how much I have allowed myself to transform from the inside out in this past year. My deepening of my inner-work has created an opening— I am more capable of holding a container for DEEP emotional journeys. Speaking Grief is a language that transcends words. The Ancestors have guided me in the Root Work, as I hear/feel it so appropriately named. It is deeper, more connected, and more relational than “standard pelvic PT.” I feel truly honored to offer this type of care and to equally report that I continue to receive deep relational healing.
Starting in 2025, I will be sharing more about my upcoming offerings around incorporating Psychedelics in the Root Work I offer. For now, I want to deeply thank all who have trusted me in their inner-work this past year. I have grown so much and I feel Rooted PT has really mirrored back to me that “Me-Care is We-Care”— which is a fundamental truth to collective healing first written about by Audre Lorde, a Black, Queer, Disabled writer, poet, and change-maker of her time, whose work has deeply influenced my offerings.
To close this— my Ironman is October 27th! I look forward to concluding this part of my journey, which will also mark 6 months since my Mom’s transition.
If you are currently a client, I would recommend booking your appointments out for the rest of the year, as my availability in November is sparse.
Thank you. I love you. Tenderly,
Grace
Transformed by Death
“Grief is an Identity Crisis” — R.C.
I am transforming.
Rachel Cargle shares, “Grief is an Identity Crisis.” Rachel recently lost her Mom and all her descriptions of the unraveling that follows resonates in my bones.
After Dad died, I was afraid that losing my Mom would break me. And in many ways, it has.
My heart hurt so bad just from grieving Dad, that I was convinced I was having a heart attack last year. After an echocardiogram and stress-test, showed a completely healthy heart, I realized how important Somatic therapy truly is. Emotional and physical pain loop together— one effects the other. Somatics is acknowledging this evolutionary connection.
Only after I learned that my heart was in fact strong enough to with-stand this, I surrendered even more to the pain of Mom’s transition.
I am unraveling, unfolding.
There are parts of me that are dying along with my parents.
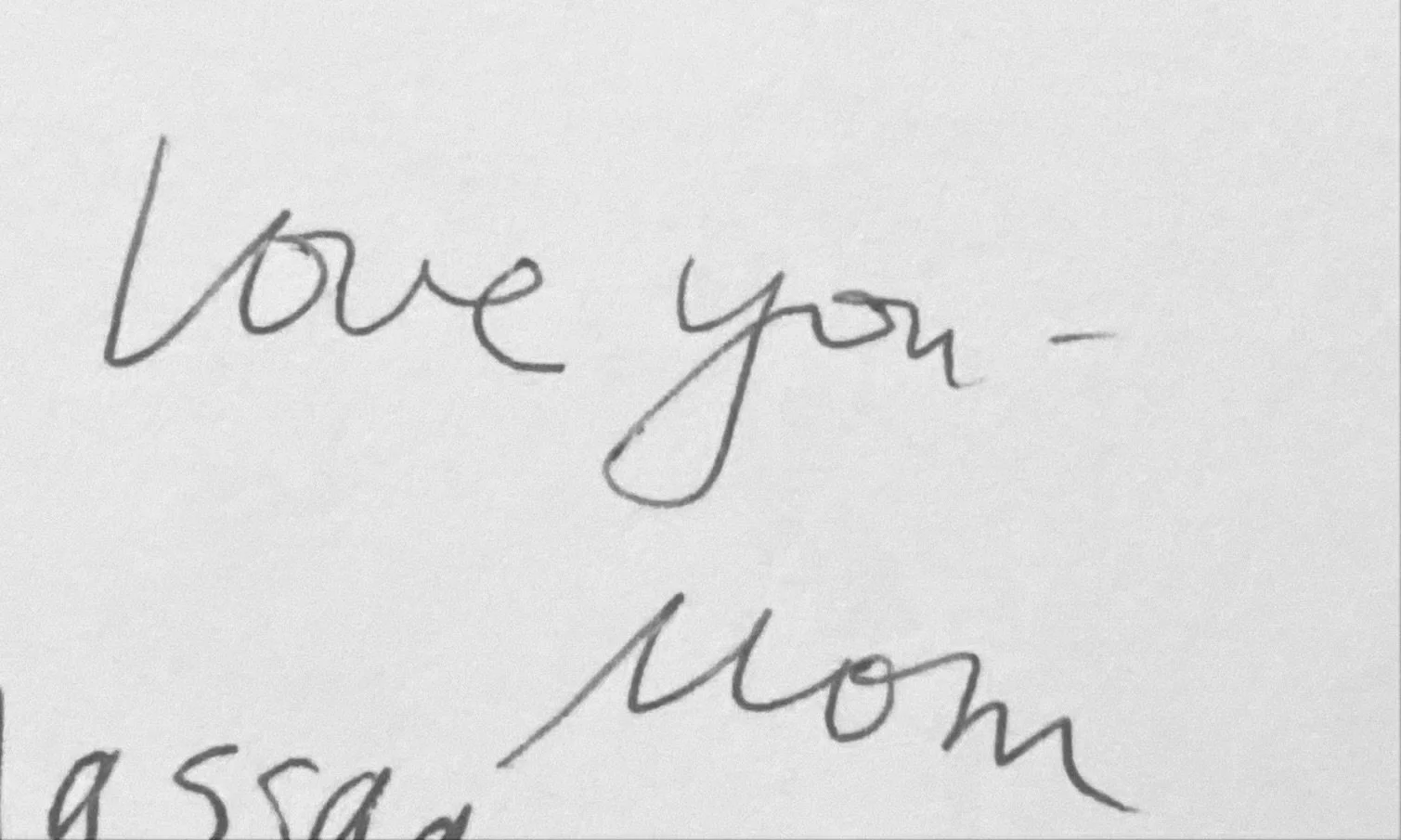
I felt the Ancestors calling me inward deep into my pelvis for some honest root work within myself since last year. I kept hearing, “Who am I?” This work was intensified and amplified by witnessing the genocide of Palestinians. The questions deepened, “Who are we?” What a tremendous amount of grief. I didn’t know how to cope, how to continue to witness what I soon learned to be multiple on-going genocides (Congo, Sudan, in fact there are I believe 14 worldly genocides presently) while my system was so pressurized.… Alexis Pauline, Rachel Cargle, Aja Monet, Dr. Jennifer Mullan, Amanda Seals, Bell Hooks, Angela Davis, Kaitlin Curtice, Adrienne Maree Brown, Prentis Hemphill — all brilliantly fierce, grounded with humanity at the forefront, versed in turning pain into power— they all guide me as true Mother-figures. The Motherly guidance that I’ve needed, came from their words, songs, and poems. I encourage you to know all of their names and buy their books/music/poetry. It’s still unfathomable to me that in the months leading up to Mom’s death, “Cease fire” and “love you Mom” were the most important words from my lips.
Witnessing. Witnessing versus bystanding. My body and this inner calling to investigate who I am lead me to confronting my internalized “bystander.”
Dr. Resmaa Menakem, healer, author and founder of Somatic Abolitionism, talks about racialized trauma, “white bodies haven’t built this agility, acuity, or grit, when they encounter strong energy or stress around race, their racialized trauma can easily get activated… shift[ing] into fight, flee, freeze, fawn, or annihilate mode. Often this means becoming anxious, or angry, or defensive, or tearful. They may then try to blow their pain through other bodies—especially bodies of culture.”
Though Dr. Resmaa’s work is not new to me, I recognized bits of it in myself even more recently— the bystander. What have I stood by and just watched? How has whiteness privileged me even in the last couple months? It took me time to really reckon with the parts of me that were confronted by my own fragility in maintaining my activism while facing profound loss. It lead me to think of all the ways I have harmed myself as my own bystander. So often, I stood by while my parents harmed me and I tried to hide it— it was a family secret. Bell Hooks talks about this hiding of abuse in homes that present themselves as loving. But ya, my truth is that I survived my upbringing by primarily dissociating, freezing, shutting down, and fawning— all of which happens in the system of a bystander. Dissociation including perfectionism, over-thinking, obsessive learning, fragmentation or numbing parts of our bodies, fantasizing or living in stories. I grew up learning how to protect the fragility of my parents and my family— taking it in as my job.
It feels clear that the bystander in me is dying along side my Mom, or at least is trying to. It’s hard to forgive myself for the times I learned truths and still remained quiet. And I need to forgive myself for the times I allowed my body, mind, spirit to be harmed by my family. Now as I look up even more, and try to take in the whole world, I’m confronted with overwhelm, rage, and grief. If I am letting go of the bystander’s way of surviving, then I am choosing to use my voice to speak Truths. The truth is that I deeply loved my Mom, alll the way down into my bones, and more truth is that she wasn’t kind to me.
As a queer kid raised in a homophobic family, I was so busy trying to survive without losing myself. But now I feel some shifting— its time to let go of the homophobia that I took into my body. Its time to let go of the transphobia that I took into my body. Those tools of destruction were never mine to begin with.
I am choosing to stay here. As my Mom and I untethered from each other, I wasn’t sure I could stay here without her. After all, who am I if not my Mom’s emotional regulator? Who am I if not my Mom’s protector?
There is freedom in that space… I get to be my emotional regulator. I get to be my protector. I get to use my body and my voice to fight for the world that is worthy of my existence. I get to rest, and celebrate and find joy. Queer people deserve to live.
My parents were very misguided. And their ideologies were enabled by Christian Theology, “Conservative” News Media, and a certain Catholic cult that doesn’t need to be named. Their behavior was accepted by too many people in their lives— including me. They dehumanized me. They held White Fragility close to protect their racism, Islamophobia, Xenophobia, Homophobia, Transphobia… My parents weaponized their fear and their shame.
Mom and Dad at their church, a month before Dad died. 7/2/22
I refuse to continue this pattern. I must break the cycle.
Thank you to some of my close friends who have called me out on my harmful ignorance and rhetoric while I was waking up to Truths and reckoning with the closed system I was raised in. In my teens and 20s, I had a lot of unchecked White Fragility. Mixed with my Autism, I had big melt downs when encountering shame for harm I caused. I learned that only someone who really loves you will trust and believe that you can and will do better. I learned how to ride shame spirals, and how tolerating it was a gift; I would come out the other end more aligned with who I know myself to be. My somatic abolition work remains at the forefront of my somatic practice. Thank you to the Ancestors for believing in me— for believing I have a role in this call to protect our children. Thank you to the children of Palestine, Congo, Sudan, both living and ancestors, who call us to overcome our limitations in order to speak up and out for their right to freedom.
I hope for more relationships that allow for corrections— authentic feelings, cause and affects, and repair. I hope for a government that starts the necessary process of reparations for a horrendous history and on-going pattern of violence and domination and greed. I hope for more people to come together on a shared vision of changing this mythical hierarchy and choosing a path of equity and equality.
The bombs need to stop.
Black, Brown, Indigenous, Asian, Arab, Jewish, Disabled, Queer and Trans kids need to be protected.
I feel deeply committed to this vision. All my gifts must go to making this place a little more accountable, kind, courageous, compassionate… I feel late arriving to a deep mission that was here way before me and will be here when I die, but there is no time like the present. What can I do now? And I think it starts with me practicing speaking more Truth.
My grief is what is driving this transformation. My feelings and my heart break remind me of my humanity, my courage, my power, my resiliency and my capacity for growth.
Now I get to see what my life could be like if I actually loved myself because of my queerness, my non-binaryness, my neurodivergency. What would it look like if I knew I was worthy of protection? How might my relationships shift?
My practice is in the healing arts— and I really identify it as my art. I’m adding more color and creativity. More truth. More authenticity. More Grace.
It all starts by breaking what I thought I knew, and uncovering my Truths. This takes time and I’m so so in it.
I can’t wait to celebrate the transformation, but for now, I grieve and I shatter so that I can be remade into who I was always meant to be.
I love you Grace. You are so incredibly worthy of this transformation. I believe in you and I’m sorry for all the pain you’ve endured on your journey home.
Grief: Part 3
Feeling the hurt and why grieving with other’s is important.
Turning towards the hurt.
So much of what I offer my clients, is a container and guidance in the form of reassuring, loving presence and attunement so that they may CHOOSE to turn towards the hurt— and that means opening yourself to feeling it.
One time, this year during my own therapy session, I just finished spending about half the session crying when my therapist asked me why I waited until our appointment to let myself cry. I was so confused by that question. Was I supposed to be able to handle this much grief and pain on my own?
I’ve learned something… no. None of us are here to endure pain alone. There is nothing to prove in managing, and working with your pain independently. It doesn’t prove strength. It doesn’t buy admiration, nor earn respect. It isn’t loving towards others nor towards yourself. We are wired for connection. Connection amplifies pleasure, love, joy, relief, gratitude, AS WELL AS rage, confusion, hurt, fear, grief. It is the connection that provides much of the healing. We have been hurt in relationship, and it is in relationship that we can find healing.
This year I needed to grieve openly and with others. It has helped me move really big energies in my body. I’ve learned more about pain and loss, enough to know that I don’t even know all of the pain and loss there is. It has helped me see more of what other’s quietly carry, and why they carry it quietly.
Is it safe here to show how much I am hurting? Will there be connection through it and in it? Can I trust you to hold me as I show you my hurting?
Yes. Yes I am here for your hurting and my hurting. You don’t have to hide it away deep inside and pretend it isn’t there. You do have a right to your hurting. Your hurting doesn’t need to be minimized, gaslit, dismissed, shamed, swallowed.
In fact, loving the hurt is what gives it space. Seeing the hurt and validating it’s presence gives it voice. And reminding it that it gets to be here too without anyone’s agenda allows it to move in and through our bodies.
A Love Note To My Body:
It’s been a year since he died. And it’s been many many years since he abandoned you. I see you. I know what you have been working on. I know why you grind your teeth at night. Why your tummy feels so tender. I know. I get it. And it makes so much sense. You’ve been grieving this loss for a lonnnggg time— even before other’s could see it and name it. And what’s worst, you were left alone with this grief in childhood. You took it in to mean there was no space for you in this world. That must have really really hurt. That must have hurt so very badly. Thanks to your resiliency, you’re here now. And the only way through is with loving yourself— you know this. So take some time off of working. Take time off of doing things. Take time off of moving through the world as if this isn’t painful and also a lot of work. Take time off of caring for others and pour into yourself. Pour into your body and your spirit. Massage the muscles that have been straining and quench your thirst. Feel the loss, anger, confusion, disgust, disappointment, grief, exhaustion. I will be here with you as you feel it. I will make space for it. I will validate it. I will love all these little parts of you and remind you how loved you are. I will prove to you that it is safe to turn towards the hurt.
I love you. I’m sorry you’re hurting. And I’m proud of you for feeling it. I’ve got you and I’ve got us. The people who love you have you too. — G
Grief: Part 2 (Blame Culture)
T.W. Death and Dying.
Since my Dad died, I feel a strong desire to apologize to every client I ever worked with before Dad died. I didn’t know then what I know now. Here’s something I have experienced and learned— we are in a grief-averse culture.
There are several strategies of avoiding grief— even from witnessing other’s grief. One is coined, “blame culture.” It sounds like…
“He had a heart attack because he was fat.”
“She lost the pregnancy because she didn’t really want the baby.”
“They just needed to face their unresolved trauma.”
“They couldn’t handle the pain, that’s why they had a cesarean.”
We’ve witnessed this Victim- Blaming strategy time and again used by Oppressive Systems and people. Like…
“If she didn’t want to get pregnant, she should have used a condom.” (note the ‘she’ pronoun is often used in this sentence)
“He shouldn’t have resisted arrest.”
“They shouldn’t have worn a short skirt.”
“She didn’t even look like she was in pain so of course the nurse didn’t take her seriously.”
“He shouldn’t have disobeyed me.”
These comments close off empathy and compassion. They put up walls between our connections. They uphold violence and Hierarchical Oppressive Systems. They give a false sense of control to the person saying it. And they really identify the real disease which is avoidance of grief and lack of empathy.
Blame Culture’s strategy sounds like— If I blame you for your grief, loss and pain, then I don’t have to acknowledge the fragility of human life.
Sometimes, we lose what and who we love. And it doesn’t make sense.
Grief isn’t bad. It isn’t something wrong that you are doing or experiencing. It doesn’t have a nicely organized “5 stages.” It’s f*king painful, and it doesn’t “go away.” It’s nothing to “get over.” You don’t need to grow from it. It takes way longer than 6 months, which according to DMS is a disorder. It’s been 6 months since Dad died, and my body STILL needs regularly reminders that I am alive and here. I still feel my chest is tight. Going to work often feels challenging— in fact, I really feel I should have had a paid year off of working entirely just to support my grieving process. But we live in a culture that pathologizes grief.
Grief is a natural response to heart break and loss. It is love in it’s most raw, wild, untamed, painful form.
There’s a part of our brain that tries to make meaning out of our experiences. Evolutionarily, this is to help us identify and avoid danger. But in some cases, there is no way to make sense out of loss. So we need to learn how to comfort that meaning-hungry part of ourselves without minimizing, rationalizing, bipassing, and victim-blaming.
There’s nothing I did or didn’t do to “deserve” my Dad dying. And I truly believe there was nothing he did. He would have told you that his Lord called for him. But the Christian theology has never brought me comfort the way it has for my parents. In fact, I have experienced lots of Blame Culture in religion.
Please watch out for this victim-blaming strategy in the reproductive, pregnancy, fertility, birthing, and parenting world. All it does is make people feel isolated with their grief.
Blame Culture phrases that I have heard:
“Did you do xyz while you were pregnant? That’s what I did to keep my pregnancy.”
“Maybe you aren’t producing enough milk because you waited to bottle feed.”
“Why are you still processing your birth? Your baby is a healthy 1 year old!”
“Maybe you were with the wrong guy. You just need to find a better match!”
“You just need to be strong.”
“This is all happening for a reason/your greater good.”
YUCKY. All of these imply that your grief is your fault. It’s not true and it’s not helpful.
What to say to someone who is sharing their grief with you:
“That sounds so painful. I’m here and your grief is welcome here too.”
“I want to be here and support you in your grief. Here’s some ways I’ve thought of that might be supportive to you…”
“I’m wondering how I can really make sure you feel that I am here for you and your grief. Would you like me to listen or a hug?”
“I just want to remind you that your grief makes sense and is important.”
“I want you to know that your grief isn’t too much for me and you don’t have to take care of me as I witness your grief.”
“I’m here for you and your grief, and I’m not going anywhere.”
“I’m noticing I am wanting to ‘problem-solve,’ and try to take this pain away for you, but I know I can’t. Instead, I just want you to feel that I am here and I love you.”
I will model this language to you as I am with you and you may notice how it opens the space between us for true healing. The healing isn’t to “make the grief go away.” In fact, it is the opposite. It is to welcome it. And ultimately to integrate it.
The Grace I was before Dad died is not the Grace you are witnessing now. I don’t feel I am better or worse— Just different. And that makes sense. I am still whole and Loved and capable.
To Grace before Dad died: I don’t blame you for not knowing about grief to this depth. In fact, I wouldn’t have wished this on you. Your grieving process is complex and layered— and that makes sense since you and Dad had a complicated relationship. Take your time with grief. There’s no “right way” to do it. I’m here for it and it’s not too much for me. You don't have to be strong or anything, but I do really honor your courage in feeling the grief as it travels with you and moves in you.
To Dad: I’m pretty disappointed that you used Victim Blaming a lot with me and around me. I learned about empathy, compassion, and equity&equality without and in-spite of you. I don’t blame you for dying. And I hope your soul is free from the restraints you placed on yourself and others while you were earthside. Love you.
Grief: Part 1 (About My Grief)
Navigating grief and the pelvis— through my journey.
For those of you who follow me on Instagram, then you know, my Dad died unexpectedly in August 2022.
So much has changed for me since then. I had to slow down and focus my energy and time carefully. So I stopped writing blog posts, and in many ways I slowed my efforts in “work” in general. My heart and my body needed more of my time and attention, and some things had to give in order to support my changing needs. Which is a natural shift that our western systems do not support— more on that later.
My initial response was a heavy Freeze response. I felt immobilized. Like I couldn’t move. I couldn’t call people back. I couldn’t think of tomorrow. I could only just hold still. Luckily with Somatic Experiencing™, I was able to shift the stuck-ness. I moved through the horror, confusion, anger, shock, and I landed on grief.
Grief.
Grief is a right of passage— a journey that we all embark on. And it doesn’t end, it just walks with us, like a companion. I’ve known grief before Dad died. Actually as a queer person to homophobic parents, I’ve known this loss of the greatest kind for more of my life than I haven’t. What I’ve learned, is how to honor my grief. Stories of “getting over,” and “moving on,” and other minimizing ideas around grief now sound completely disillusioned. I am waking up to our societal resistance to grief. At the time of Dad’s death, I was working per diem at Kaiser Permanente. They offer 2 days of bereavement leave— unpaid. Meaning, they expect their employees to come right back to work 2 days after such a loss. And we call this healthcare? It was so clear that I needed to once and for all, remove myself from the broken system of healthcare.
Grief and the pelvis.
Grounding while grieving takes intention. Grounding includes sensing into both my internal and external landscape.
What feelings are with me today? What’s here that needs my attention? How’s my water intake? How’s my sleep? Hows my nervous system navigating this?
In order to really tune in to myself as my body/mind/spirit processes that my Dad is no longer earthside, I have had to really acknowledge the areas in my life where my boundaries are built on quicksand.
What policies in my practice do I still hesitate or feel insecure in reinforcing? How do I want to spend my time? How do I want to make money for my expertise? What happens inside myself when someone pushes back on my boundaries?
This is the pelvic connection. When I step out of myself, when I abandon my wants and needs, in order to protect “the connection,” then my pelvis feels and experiences my internal betrayal to Self. My pelvic muscles tighten up which has given me hemorrhoids (boooo!) The self love I need in order to survive this time in my life needs to be RADICAL.
I can only treat 4 clients a day, and I need to charge enough for this to be sustainable. I need nature. I need connection with people who truly love and value me. I need my “No,” to be enough without excessive explanation.
Interesting thing about navigating death and dying, is how much of a daily reminder my body needs that I am alive and worthy of love. My body, My pelvis need to hear from me multiple times a day— that I am alive and here and loved.
If you have continued to work with me during this stage in my evolution— THANK YOU. Thank you for trusting me to take care of myself and my grief enough to be able to take care of you. Thank you for valuing my skills/expertise. Thank you for being seen by me, as well as for seeing me. Thank you for not comparing our suffering (this goes in the useless category along with “get over it,” “move on,” and “time heals.”) I believe in what I offer not just as a human to humanity, but also as a healer.
To Little Grace: I have your back— forever and always. I cherish you and deeply love you.
To Present Grace writing this post: I believe in you. I trust you. I can’t wait to see you continue to live and feel/experience your aliveness. Your grief is welcome to stay so unclench your butthole, and instead plant your feet lovebug.
To Dad: Your fear for me never helped me, in fact it hurt me. You don’t have to be afraid for me anymore— not of where I live, of who I love, of how I identify, of how I make money, or of how I connect with Spirit. I picture you letting go of your fear and resting. And all I can tell you, is that I’m here trying to do the same— letting go of fear, and turning towards rest instead.
Granular Tissue in the Vaginal Wall— What To Do About That?
Granular tissue in the vaginal walls and what to do about it.
Granular tissue is a type of tissue with contractile properties that forms in tissue healing that is prolonged. For example, if part of the vaginal wall tears during childbirth, and the edges of tissue are not sutured (surgically repaired/approximated), then granular tissue will form and close the wound from the deepest layer first. This tissue is often tender/painful, inflamed and has many capillaries or dense blood flow.
It is incredible that our tissues are capable of healing the vaginal wall through this tissue growth, however, the slowed healing and tenderness of the tissue may contribute to vaginal pain and discomfort.
To support healing of these tissues, rest, nutrition, hydration and stress management are all important. If a post-partum person is chest feeding or pumping, then keeping up with the body’s need for replenishment of nutrients and rest is even more important. I have seen this slowed healing present in bodies that are under-fed, under-hydrated and under-slept— in general under-supported.
Unfortunately maternal health is not supported through our country’s politics, nor monetarily. So post-partum people often do not have adequate resources, paid-leave, childcare, and physical healing support in a time that the body really needs these basic human rights for care.
The message one could take from this is that birthing people’s recovery does not matter— and I urge you to NOT take this into your body as truth. It is a lie. Your healing matters. In fact— it matters the most!
Here are some ways you can prioritize your own healing in the postpartum period:
Take a bath before bed. Just as we wind our babies down with a comfort routine before bed, your body would benefit from this nightly routine as well. Maybe use epsom salt or healing herbs. ( I recommend Peri Soak) This floating bath supports tissues healing, nervous system relaxation, and therefore muscle relaxation necessary for rest.
Drink plenty of water. It is often recommended to drink half your body weight (in pounds) in ounces of water. For example, I weigh 190 pounds, and therefore should be drinking 80 ounces of water daily. Now if you are producing milk, add the water necessary for that on top of that number! Wow that is a lot of water… yep! You need this much for your hydration.
Allow rest. Many doulas and midwives in my community tell their postpartum peeps to rest or sleep whenever baby is sleeping… that is not wrong. Your body needs rest to heal just as much as your baby needs rest to grow! I recommend Yoga Nidra as a rest practice as it helps your brain enter healing wave lengths and patterns. Try Insight Timer and search for guided meditations on Yoga Nidra.
Pelvic Physical Therapy: In one session we can determine if your muscles are needing active or relaxation types of exercise to support healing. You may also need to be referred for a fitting of a pessary which is an internal support device. You may need internal tissue manual therapy to support healing or there may be some stored trauma that needs attention and a chance to integrate to support healing.
Cauterization. If the granular tissue continues to be a source of pain and discomfort, you can ask your OBGYN to cauterize the tissue, meaning they will use a chemical to burn off the tissue. Make sure your physician uses a topical lidocaine gel or injection prior to removal of the tissue. This is a simple outpatient procedure, that may result in minimal spotting for a day or so following the treatment. Please discuss with your OBGYN if this is appropriate for you.
Legs up the wall. If your pelvis is feeling like is could use some support, try lying with a pillow under your sacrum and your legs supported up on a wall. Allow your breath to deepen and massage in the inside of the pelvic bowl and imagine you and your pelvis being held and supported by all the people in your life who love you. Allow yourself to receive the message that your healing is the most important, and your pelvis is in fact loved and supported by many.
Witnessing and being a part of your healing helps me remember that my healing too is valuable. If I didn’t prioritize my own rest, hydration, and stress management, then I wouldn’t be available to help all of my clients. So I don’t take in the messages from systems that say anything to the contrary.
You are so so loved. And your pelvis is held up by all of us.
Kegels.
Let’s talk about “kegels.”
Arnold Kegel, born 1894, was an American Gynecologist and just one of the MANY CIS White Male Gynecologists experimenting and learning on many female bodies, especially Black, enslaved female bodies.
The term, “kegel,” is one of many terms and names used on the vulvovaginal and uterine/ovarian bodies that are named after White Men. To reclaim our bodies in name and with language, I prefer to no longer use the term, “kegel.”
When people refer to a kegel exercise they are describing the concentric contraction of the pelvic floor diaphragm muscles (it is not a floor.) The problem with this is that the vast network of muscles moves both concentrically (shortens) and eccentrically (lengthens) and both movements are important for pelvic health.
We often find these muscles activated concentrically (shortened) when in a state of stress. If your body is guarding or bracing, it may contract certain muscles around VITAL organs to keep us alive. You can imagine what your neck muscles would do if you saw a car heading towards the back of your car at full speed. They tense up in an effort to protect your brain and neck! That is a reflexive reaction that is developed over thousands of years of evolution towards our survival.
So now, if we bring that same intelligence to the pelvis— it is easy to imagine what those muscles are tensing up for! If we ignore this, and then send a repeated message to contract and shorten with the KEGEL exercise in order to treat ANY pelvic condition then we are MISDIAGNOSING and MISTREATING the pelvis.
It wil important to attune to the pelvis and to our bodies as a whole. To ourselves as whole. Do the pelvis muscles have mobility? Do they move up (in) and down (out)? Do you know where they are right now in the moment? Can you concentrically contract them? Eccentrically contract them? Can you hold that contraction while you breathe deeply? Can you contract them quickly? Can you release them quickly?
>> After all that, do you still feel comfortable talking about them as kegels? I would think not!
Kegels don’t solve pelvic issues. Pelvic Awareness, Movement, breath, coordination, endurance, power, speed, mobility, and strength will feel most supportive… and that is why I call them Pelvic Exercises. <3
Do I Need Pelvic Support During Labor?
Labor pelvic support for the birthing person.
A case review:
Mama called saying her labor started 4 days ago, and “water broke” 28 hours ago. She said the cervix checks were painful and so her midwife was unable to get a good check in on cervical dilation. She asked me to come over to see what I could do to help.
We discussed the benefits and risks of Direct Pelvic Diaphragm work ( intervaginal/ interrectal) and both agreed to work indirectly on the pelvic area (outside of the pelvis). When I arrived, labor was stalled with contractions >10 minutes apart. I noticed the sacrum (pelvic bone and fused segment of spine) was rotated to the right, the right> left hip flexors (muscles) were restricted, the cesarean scar tissue was pulling on the left round ligament, and the posterior pelvic diaphragm muscles were guarded/restricted.
As I worked on manipulating the sacrum, releasing the scar tissue and pelvic diaphragm, Mama and I discussed how the pressure/discomfort she was feeling in around her anus was a good sign and we worked to find ways to support her into moving IN TO and With that discomfort, rather than resisting it.
We both talked to Baby, encouraging him and asking him if there was anything he needed.
One hour later, Mama was in ACTIVE labor. We both felt her baby move his hand away from his face and rotate his head down low into the pelvis. I supported Mama in finding a birthing rhythm and strategy to support movement with the contractions.
After the two hour mark, the Birth Doula arrived, and I headed out sending everyone my love.
The midwife arrive 2 hours later, and shortly after Mama had the V-BAC she dreamt of.
I am so grateful I was able to assist this team in supporting this Powerful Mama in Labor.
Wondering if this type of support is right for you? Read more about it here.
Is It Your Hip or Ovary?
Hip or Ovary pain? Let’s talk about how the two relate!
Are you experiencing pain in your hip or lower abdomen? How do we know if it is pain coming from your ovary or hip?
Hip Dysfunction often refers to the lower abdomen, leg, low back, groin and even the ovary.
Ovarian Dysfunction often refers to the same areas— so which needs the attention?
Here are some thoughts:
Your ovary may be the “source” of pain if your symptoms are worsened around ovulation and bleeding times in your cycle.
If you have a history of ovarian cysts, PCOS, endometriosis, anovulation, then you may want an ultrasound screening of your ovary.
If your hip has limited, or painful movements, then you may have more of a hip issue to work with.
Often, back pain is caused by hip mobility issues! If your hip is unable to move or stabilize your pelvis, then your back will take on the compensations and strain.
Hip issues often lead to over active hip flexors, which is the muscle that inserts on the front of the hip near the groin crease. Hip Flexors are a powerful muscle group of the illiacus and psoas, combining to illiopsoas. These muscles run along your spine, starting from the base of the respiratory diaphragm, and inserting at the top of the hip. These muscles will support you in a fight, flight and freeze response. So if your body is experiencing a stress response, these muscles may be the first to engage in protection.
In an evaluation— we first will screen your hip movement, then we will screen your ovary movements. This will inform our course of treatment.
On your own— try massaging your ovary, and your hip to start to self-exam the two. Notice if you consistently cross one leg over the other or carry your kiddos on one side. Notice if your symptoms are constant or cyclical. Offer your body some hip mobility and breath exercises as demonstrated below.
Pelvic Healing After Cancer
Pelvic healing after cancer— Your pelvis may need care after common cancer treatments and pelvic physical therapy can help.
Too many patients are not referred to pelvic health following cancer treatments. Unfortunately, radiation, surgery, and chemotherapies can have a profound impact on pelvic health and sexual health. Some treatments include removal of pelvic organs including the colon, bladder, uterus, ovaries, testicles, and prostate. In addition, the pelvis may go through transitions such a early menopause.
Cancer is hard enough— navigating pelvic health during and after treatment deserves support from a professional. Here are some common complaints:
Bladder changes may occur either due to a neobladder , urostomy, prolonged catheterization, prostatectomy, or radiation to the pelvis. Common complaints are difficulty releasing a stream of urine, urgency (rushing to pee), increased frequency of peeing, pain with peeing, leakage of urine.
Vaginal Pain may occur with radiation, or early onset menopause from hysterectomies. The vaginal tissues may become dry, hypertrophied, sensitive to touch and prone to tearing. Sex play including both vulva focused and vaginal focused touch may become painful. I often see trauma from fighting and surviving invasive surgeries impacting sexual relations between partners.
Testicular and penile pain, pain with erection or difficulty with erection/ejaculation may be experienced after treatments.
Bowel changes may occur as the colon adapts to changes within the pelvis. Common complaints are slowed motility, difficulty emptying, soiling or leakage, urgency, or changes in frequency.
Here’s how physical therapy interventions support pelvic healing:
Treatments may include scar tissue management, fascial mobility with manual therapies, pain management, bladder or bowel retraining, pelvic muscle training, trauma response integration, sex-ed, movements/exercises to support whole body mobility, balance, and regulation, etc. To read more about the specific interventions I offer or on my advanced training, read here.
Mostly, I want you to know, your pelvic health is important. Healing is available to you. There are resources for you and your love ones as you navigate the hardships that often come with cancer treatments.
You are so precious and loved and you deserve to feel peace and pleasure in your pelvis.
Clogged Milk Ducts
Tips for chest feeding/ breast feeding people in support of reducing clogged ducts. Free shoulder mobility video included.
Many chest-feeding people don’t know that physical therapy interventions support motility of milk.
Heard of ultrasound therapy? It basically vibrates tissues and has good evidence in supporting movement of milk. You can read more about it here. You can buy your own ultrasound machine for your home use! They run about $30-80.
Oralfacial and tongue mobility of Baby in addition to the feeding position can support chest/breast health. I love craniosacral therapists for this kind of support!
Water intake is vital! Whatever amount of milk you are producing, you need to take in enough water to cover that PLUS water for your own systems. A non-milk producing person, needs about have their body weight (pounds) in ounces of water. 180 pounds, is about 90 ounces of water intake.
A practice of stretching the chest, mobilizing the shoulders, and deep breathing can support a reversing of the cradling/feeding position.
There is support for you! Making ALL the meals for a hungry-growing baby can be overwhelming and isolating— but you are NOT alone. We see you and love you.
Bladder Hygiene
Or should the title be “HOW TO PEE 101” ?
Here is the PEE info you never got—
Don’t Pee “Just in Case” If you teach your family, and yourself to pee before you go, then your bladder will learn this behavior and potentially hold you to it! Your bladder is meant to tolerate holding urine comfortably for 2-4 hours.
Typically we want to see 6-8 pees per day, and 1 per night. If you are peeing 1x/hour or less than that— it is time to book an appointment! That would be considered increased bladder frequency. Things that can affect this, include diuretics (medicine or caffeine that make you pee), irritants (some citrus/juice/coffee/alcohol/sugar/carbonation), or behaviors (see #1).
SLOW DOWN to pee. If you are rushing to the bathroom, and trying to push down to “pee faster,” then you in general are moving too fast. Take some deep breaths. You should be able to slowly walk to the bathroom, slowly remove your undergarments, slowly release your pee until completion.
Feeling like you can never empty your bladder? Well perhaps get tested for urine health, and if the feeling persists— time to see a PT. The feeling of a UTI can linger as tissue memory from the nerves, muscles, fascia and feeling fully empty might be a struggle. If you are in fact needing to empty again shortly after peeing, you may also be experiencing symptoms of prolapse— WAIT! Don’t freak out just yet. This is a possibility- not a Dr. Google Diagnosis time… so be sure to take a deep breath, and see a PT!
Does a full bladder or peeing hurt? OK time to see a PT again. Holding urine, releasing urine, should never hurt. This can be do to a number of things… best to get checked out.
“I was told to practice my kegels while peeing to see if I can stop the flow of urine.” DON’T DO THAT. That was BAD Rubbish advice that was spread during my Mama’s generation.
“I was told holding my urine in would give me a kidney infection.” A Catheter increases risk of infection. Wearing a penis-clamp (if you don’t know what it is— it’s what it sounds like) for too long could increase a risk of harm. But holding a full bladder for 2-4 hours… now that is harmless. Imagine being on the window seat during a plane, or in a long movie, or SLEEPING… holding in urine is okay. Side note— I would still encourage peeing after a sexual play session involving vaginal penetration, or bacterial exchange around the urethra (aka touch without a dental dam or condom).
LEAKAGE IS NOT NORMAL. Ever. Not at any age ( above 4ish years old). Not during or after pregnancy. If you pee you pants (even a little) when coughing, sneezing, washing dishes, running, jumping, hiking, during sexual play (different from golden showers and squirting), then seek pelvic PT.
Odds are— you’re dehydrated. MOST people I see are dehydrated. Try to drink half your body weight in ounces of water. Since I weigh 180 pounds currently, that means I should have a goal of 90 ounces of water intake. If you exercise, make milk (with your chest/breast), talk a lot (like a teacher), then you might even need a little more. Can I drink too much water? YES. Yes actually. There is a sweet spot for hydration. And no, coffee, beer and soda do not count for hydration.
Blood in your urine? Call your Medical Care Provider immediately… that isn’t normal.
Menstrual Cups
Why does my menstrual cup fall out? Learn about menstrual cups and pelvic health.
Is Your Menstrual Cup Falling Out? Here’s Why
Your menstrual cup is shaped to create a suction cup around the cervix, however, it keeps it’s seal by resting on the pelvic floor muscles. There are a couple of reasons your pelvic floor muscles may not be supporting the menstrual cup.
The pelvic floor or diaphragm is a group of muscles on the underside of the pelvis responsible for supporting the bony pelvis, the internal organs including the vagina, bladder, and rectum, and support sexual functions. Pelvic floor dysfunction or problems with the muscles of the pelvic floor includes decreased strength, restricted tissues, muscle spasms, or overactive muscles. There are several reasons you could be experiencing pelvic floor dysfunction including vaginal or cesarean birth, trauma, anxiety and stress, constipation, or something as simple as sitting in the car for many hours in the day, to name a few. If you do have pelvic floor dysfunction, some other symptoms you may be experiencing includes pain during sexual intercourse, or pain with insertion of the cup, difficulty reaching orgasm, a feeling of pressure or “falling out” in your vagina or rectum, or leakage of urine, feces or gas.
The good news is that these are similar to other muscles in the body in that they are fairly easy to assess and rehabilitate. The not so good news is that the treatment approach is not as simple as, “just do kegels” or “stop your flow of urine when peeing.” The problem is, if you begin pelvic floor strengthening exercises, but you fall under the “overactive pelvic floor muscles” category, then your exercises will not make a change in your strength leaving your cup to continue to fall out or worse, you may develop pelvic pain.
To learn about your pelvic floor, I recommend seeking professional help from a physical therapist specializing in pelvic health. You can find a physical therapist in your area here http://pt.womenshealthapta.org/
If you do not have access to a pelvic physical therapist, follow my instagram account for additional education.
Content contributed by Dr. Grace Abruzzo PT, DPT, CAPP-OB/Pelvic, CD(DONA), PYT-C
Dr. Grace practices integrative pelvic physical therapy in Los Angeles and is certified in obstetric and pelvic health through the American Physical Therapy Association.